
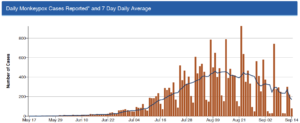
 Welcome declines in MPV diagnoses obscure spikes in parts of the U.S.: As of September 16, 23,499 people had been diagnosed with MPV in the U.S. Since early August, MPV diagnoses have fallen by 40% nationally. In Georgia, one of the states most affected by MPV, new diagnoses fell by 38% in one week. However, CDC notes that new diagnoses are still on the rise in parts of the U.S. It is unclear whether trends in new diagnoses align with trends in actual infections (see story on MPV research agenda below).
Welcome declines in MPV diagnoses obscure spikes in parts of the U.S.: As of September 16, 23,499 people had been diagnosed with MPV in the U.S. Since early August, MPV diagnoses have fallen by 40% nationally. In Georgia, one of the states most affected by MPV, new diagnoses fell by 38% in one week. However, CDC notes that new diagnoses are still on the rise in parts of the U.S. It is unclear whether trends in new diagnoses align with trends in actual infections (see story on MPV research agenda below).- Racial and ethnic disparities in vaccination persist: Distrust of the medical and public health establishment is one of many factors contributing to low MPV vaccination rates in Black communities, according to an article in the Washington Post.
- Various strategies are being used to improve vaccine uptake and equity: Demand for MPV vaccination is softening, leading CDC to launch a pilot project to bring vaccination to community clinics and smaller events. This project, which specifically focuses on improving access among Black and Latinx gay/bisexual men, is now accepting applications. A new analysis by the Kaiser Family Foundation finds considerable variation in state MPV vaccine eligibility requirements across the U.S.
- Questions about MPV treatment remain: Federal officials say that the MPV strain currently circulating in the U.S. is only a single mutation away from potentially rendering TPOXX ineffective as a treatment. Out of concern about the possibility of drug resistance, CDC issued guidance recommending that TPOXX, the only available treatment for MPV, be reserved for people at risk of severe complications, including people with compromised immune systems from unsuppressed HIV infection. Some HIV community advocates disagreed with the CDC’s guidelines, arguing instead that TPOXX should be made broadly available. A new NIH clinical trial has launched to evaluate the effectiveness of TPOXX for the treatment of MPV; TPOXX has been approved by the FDA for the treatment of smallpox and is believed to be effective for MPV, although no study of TPOXX’s effectiveness for MPV has previously been conducted.
- New evidence emerges about the health consequences of getting MPV: Los Angeles health officials reported the first MPV-related death confirmed in the U.S. CDC reported on two individuals in whom MPV infection was linked to neurological complications. As one CDC epidemiologist notes: “This is a reminder that this is not a mild illness. It can be quite serious.” MPV cases in North America, Latin America and Europe are experiencing symptoms that often differ from those reported among people diagnosed in African countries where MPV has long been present.
- Data gaps undermine our public health response to MPV: An extensive story by the New York Times describes the under-investment in public health and a lack of coordination on data exchange between federal, state and local health agencies. Without timely, granular data, including information on the race/ethnicity of people who are getting vaccinated, health leaders are often flying blind when trying to respond to MPV.
- Isolation after an MPV diagnosis is necessary but challenging: People who are diagnosed with MPV not only can experience considerable pain and discomfort as a result of the disease, but the need to isolate until all lesions are healed can result in a loss of income, sometimes for weeks.