
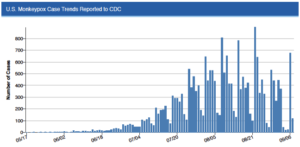
 MPV cases continue their modest decline: Nationally, 21,894 people had been diagnosed with MPV in the U.S. as of September 9. New MPV diagnoses have continued to trend downwards for the U.S. as a whole, although epidemic trends vary around the country, with some states and cities seeing faster declines than elsewhere.
MPV cases continue their modest decline: Nationally, 21,894 people had been diagnosed with MPV in the U.S. as of September 9. New MPV diagnoses have continued to trend downwards for the U.S. as a whole, although epidemic trends vary around the country, with some states and cities seeing faster declines than elsewhere.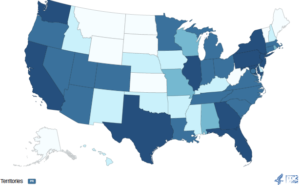 MPV cases are still high and are affecting every part of the country: High rates of MPV are occurring in every region of the country– in the Northeast (especially in New York), the Midwest (especially Illinois), the South (especially in Georgia, Florida and Texas), and in the West (especially in California and Washington State). In a review of data from eight jurisdictions, CDC found that 38% of people diagnosed with MPV were living with HIV and that 41% had a history of having one or more STIs.
MPV cases are still high and are affecting every part of the country: High rates of MPV are occurring in every region of the country– in the Northeast (especially in New York), the Midwest (especially Illinois), the South (especially in Georgia, Florida and Texas), and in the West (especially in California and Washington State). In a review of data from eight jurisdictions, CDC found that 38% of people diagnosed with MPV were living with HIV and that 41% had a history of having one or more STIs.- Health officials are investigating deaths possibly linked to MPV: Many people diagnosed with MPV experience mild or moderate symptoms, but MPV can also be extremely painful, in some cases requiring hospitalization. MPV symptoms can be especially severe among people with compromised immune systems, including people living with HIV who are not virally suppressed. Los Angeles County is investigating to determine whether MPV contributed to one death – the second person diagnosed with MPV who has died in the U.S.
- Vaccine supplies continue to improve: Increased use of the intradermal method of giving the MPV vaccine (that is, between layers of the skin, which requires less vaccine than the traditional subcutaneous vaccination) is stretching the supply of the vaccine. New York City, for example, announced 16,000 new vaccine appointments for this week and is also now welcoming walk-ins for people who are getting their first dose.
- But intradermal vaccination isn’t for everyone: A federal review of available data found that intradermal vaccination is likely to be as effective in preventing MPV as subcutaneous vaccine administration. However, people with a history of keloids (scarring) are advised to avoid intradermal vaccination. As Black people are 20 times more likely than whites to experience keloids as whites, many Southern states are relying on subcutaneous vaccination for Black people who receive the vaccine.
- Vaccine inequities persist, as those who need the vaccine the most are least likely to get it: CNN reviewed available data showing that while Black and Latinx gay/bisexual men are at greatest risk of getting MPV, they are much less likely than white gay/bisexual men to receive the vaccine.
- There is more data on MPV treatment: A CDC study found that most people with MPV who receive treatment with TPOXX experience no or very limited side effects, and that improvement in clinical symptoms took three days on average.
- Community advocates call for urgent action to address shortcomings of MPV response: The Fenway Institute released a major report outlining the public health failures that allowed the continued spread of MPV. Among of Fenway’s major recommendations is for the federal government to use the Defense Production Act to address vaccine shortages and to partner with community groups to help close racial/ethnic inequities in vaccine access.